Cardiovascular Disease - The Patient Journey
What is cardiovascular disease?
Cardiovascular disease is the world’s leading cause of death, those who have suffered it have undergone a life-changing experience. In this article, we will unveil the threats that patients experience after surgery and how those could be mitigated whilst increasing the sustainability of our healthcare systems.
What is cardiovascular disease?
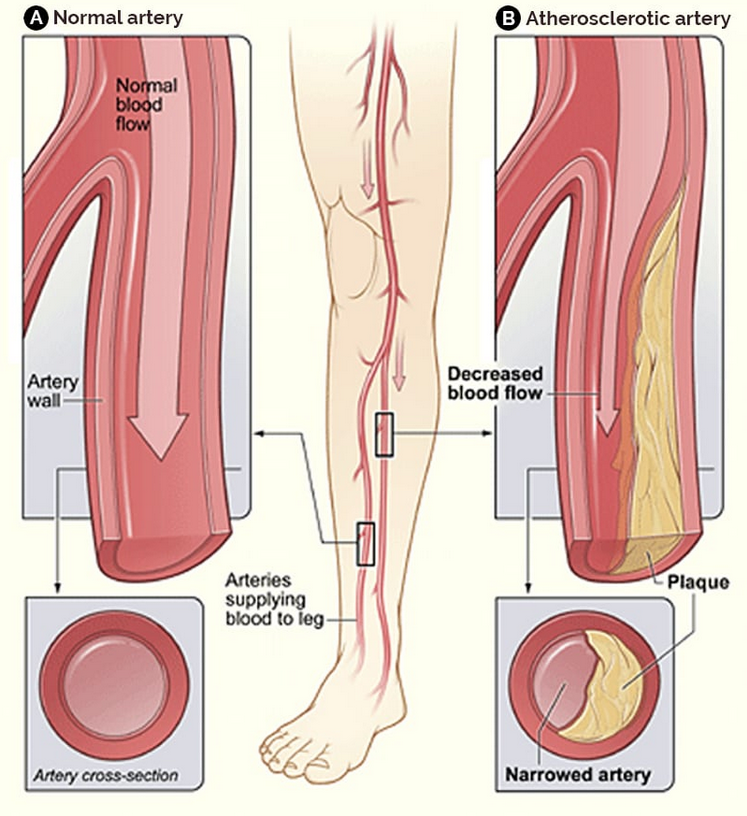
Irrespective of the vascular bed involved, atherosclerotic disease is at the basis of all occlusive cardiovascular pathology. It is typically a multifactorial disease, with risk factors such as hypertension, diabetes, smoking, hypercholesterolemia, genetics among others playing a central role.
Ultimately, these risk factors contribute to the build-up of fatty deposits within the arteries, the process known as atherosclerosis, which narrows and hardens the arteries, restricting blood flow. Over time, this can lead to a number of cardiovascular complications and increase the risk of fatal complications such as heart attacks and strokes.
One of the more common complications of atherosclerosis is peripheral arterial disease (PAD), which has major quality of life implications for patients involved. It is also a good surrogate marker for coronary artery disease (CAD) and the potential risk of stroke.
CARDIOVASCULAR PATIENT JOURNEY
The patient journey for someone who has suffered a cardiovascular event, such as a heart attack or stroke, is a critical and carefully managed process within a hospital and is composed of several steps
Patient Admission
Patient is admitted to the emergency unit
Surgical Intervention
Disease is addressed
In-Hospital
Recovery
May include ICU Recovery
In-Hospital
Imaging Surveillance
Assessment data is uploaded to the cloud
Imaging & Re-Intervention
Vascular problem detected: Confirmatory CT Scan / MRI and 2nd surgery
- Patient Admission
- Surgical Intervention
- Recovery & Discharge
- Follow up Medical Visits
- Confirmation & Reintervention
Patient Entry Into The Medical System

The patient has suffered an acute/chronic vascular event and a relevant treatment algorithm will be initiated. The patient will be admitted to the hospital where a diagnosis and treatment plan will be established.
Preparing for surgical intervention
As the plan of care is determined, the patient will be prepped for a surgical intervention. Those interventions can be minimally invasive or conducted by open surgery. A thorough evaluation on the severity of the condition will be conducted and based on best evidence, appropriate care is offered.
During the intervention the doctor will open the vessel which has been obstructed using the most appropriate tools available and the vessel will be repaired with the intention of re-establishing flow.
Patient Recovery After Vessel Intervention
Once the vessel has been reopened, the patient will be transferred to the appropriate unit for recovery, where they will be closely monitored until discharge is deemed suitable.
Preventing Re-intervention Through Continuous Checkups
After the first vascular event, those patients will be of high risk, with extreme likelihood of suffering a second vascular event in the upcoming 5 years after surgery. That means the treated vessel will restenose (renarrow) over time and most of these events pass unnoticed until it is too late.
Therefore, a medical follow up after surgery is paramount to preserve the patency of surgical intervention and avoid the complications of failure. Several medical visits with the surgeon will be scheduled during the first year to closely monitor the vessel treated.
Confirmation Of Vascular Events To Schedule 2'nd Intervention
In case a second vascular event occurs, normally it progresses very rapidly. At this point the patient is remote from the doctor’s direct supervision. Dependent on symptoms and consequences of subsequent cardiovascular events, the patient will likely be re-admitted by the hospital and a second intervention in the operating room will be scheduled.
1. Patient Admission
The patient has suffered an acute/chronic vascular event and a relevant treatment algorithm will be initiated. The patient will be admitted to the hospital where a diagnosis and treatment plan will be established.
2. Surgical Intervention
As soon as the plan of care has been determined, the patient will be prepared for a surgical intervention. Those interventions can be minimally invasive or conducted by open surgery. A thorough evaluation on the severity of the condition will be conducted and based on best evidence appropriate care is offered. During the intervention the doctor will open the vessel which has been obstructed using the most appropriate tools available and the vessel will be repaired with the intention of re-establishing flow.
3. Recovery & Patient discharge
Once the vessel has been reopened, the patient will be transferred to the appropriate unit for recovery, where he will be closely monitored until discharge is deemed suitable.
4. Follow Up Medical Visits
After the first vascular event, those patients will be of high risk, with extreme likelihood of suffering a second vascular event in the upcoming 5 years after surgery. That means the treated vessel will restenose (renarrow) over time and most of these events pass unnoticed until it is too late. Therefore, a medical follow up after surgery is paramount to preserve the patency of surgical intervention and avoid the complications of failure. Several medical visits with the surgeon will be scheduled during the first year to closely monitor the vessel treated.
5. Confirmation and Re-intervention
In case a second vascular event occurs, normally they progress very rapidly. At this point the patient is remote from the doctor’s direct supervision. Dependent on symptoms and consequences of subsequent cardiovascular events, the patient will likely be re-admitted by the hospital and a second intervention in the operating room will be scheduled.
LIFE THREATENING PROCESS
It is important to underline that atherosclerosis is a progressive disease and consequently the hazard of a repeat cardiovascular event is considerable. Surgical management of a cardiovascular event is simply fixing the devastation imposed by atherosclerosis, it does not indicate a reversal of the disease. Therefore, follow-up is imperative in maintaining the benefit of the surgical intervention and prevent the potential complications of eventual failure.

FUTURE INNOVATION
Indeed, the emergence of new and promising medical devices that offer continuous remote monitoring has the potential to revolutionize patient care. These innovative technologies can significantly enhance early diagnosis and greatly improve the prognosis for individuals at risk of vascular diseases, even before the conditions fully manifest. By providing real-time data and timely alerts, these devices empower healthcare professionals to take proactive measures, ultimately leading to better patient outcomes and a brighter future in the battle against cardiovascular diseases.
Sustainable HealthCare System
Cardiovascular disease claims a significant share of Medicare’s annual budget, attributed not only to the costly surgical equipment required for treatment but also to the potential for multiple life-threatening vascular events in a patient’s lifetime. The implementation of remote monitoring devices holds the promise of averting these severe and life-threatening surgeries. Additionally, such technology can streamline the numerous in-person outpatient clinic follow-up visits patients typically undergo during the course of critical first year post-surgery. By emphasizing prevention and early intervention, these innovative devices have the potential to revolutionize cardiovascular care, reduce healthcare costs, and improve patient outcomes.

The information published in this Blog article, or in IntelVasc Inc. website, is provided for information purposes only and does not and cannot be considered as a consultation, treatment, therapy, or medical or clinical prescription, nor is it a substitute for treatment, diagnosis, therapy, or supervision by a healthcare professional. The information published is neither intended to be used as a guide and should not serve nor be used as an exclusive orientation for the healthcare professionals to make decisions about the treatment and therapy of their patients, nor does it replace the healthcare professionals’ criteria. IntelVasc Inc. makes no warranties as to the accuracy, suitability, or completeness of the information provided, and shall not be held responsible for any decisions made based on the information provided on this Blog article, IntelVasc Inc. website or any other websites linked or referenced in IntelVasc Inc. website.

